Walking through the grocery store, Mark paused in front of the salt display, his cart already filled with colorful vegetables and lean proteins. At fifty-eight, his recent doctor's appointment had delivered a sobering message: his blood pressure had crept into dangerous territory, and his weight had become a significant health concern. Like millions of adults worldwide, Mark faced the interconnected challenges of weight management and blood pressure control—a dual battle that requires understanding their intricate relationship.
The human body operates as a complex biological system where weight and blood pressure engage in a continuous dance. Every extra pound of body fat necessitates additional blood vessels to supply oxygen and nutrients to these tissues. This expanded circulatory network forces the heart to work harder, pumping blood through miles of additional capillaries. The increased workload creates greater pressure against artery walls, much like pushing water through an expanding network of hoses requires more force. This mechanical relationship explains why weight gain often precedes elevated blood pressure readings.
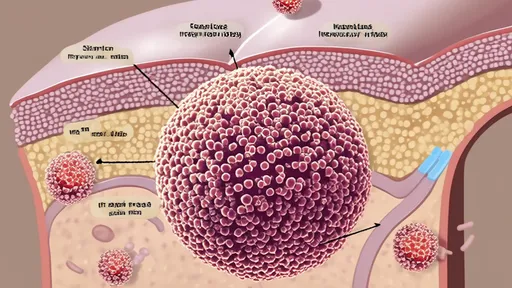
Beyond mere mechanics, adipose tissue—particularly the visceral fat surrounding abdominal organs—functions as an active endocrine organ. It secretes inflammatory substances and hormones that directly interfere with blood pressure regulation. These biochemical signals can cause blood vessels to constrict and promote sodium retention in the kidneys, further elevating pressure within the cardiovascular system. The relationship becomes cyclical: high blood pressure can make physical activity more challenging, leading to further weight gain, which then pushes blood pressure even higher.
When Sarah committed to losing thirty pounds after her hypertension diagnosis, she discovered that dietary changes offered her most powerful tools for managing both weight and blood pressure simultaneously. Rather than following restrictive fad diets, she learned to build her meals around whole foods that naturally support cardiovascular health. The connection between nutrition and blood pressure extends far beyond sodium reduction, encompassing a sophisticated interplay of nutrients that affect vascular function, fluid balance, and metabolic health.
The sodium-potassium balance represents one of the most critical nutritional factors in blood pressure regulation. Modern diets typically provide excessive sodium while delivering insufficient potassium. This imbalance causes the body to retain fluid, increasing blood volume and consequently, blood pressure. By shifting focus from merely limiting salt to actively increasing potassium-rich foods like sweet potatoes, spinach, beans, and bananas, individuals can help restore this essential balance. Potassium works by helping the kidneys excrete excess sodium while relaxing blood vessel walls, creating a dual antihypertensive effect.
Magnesium-rich foods contribute significantly to vascular health by promoting blood vessel relaxation. Almonds, spinach, black beans, and avocado provide this essential mineral that acts as a natural calcium channel blocker, helping to prevent the excessive contraction of smooth muscles in artery walls. Similarly, calcium from dietary sources like yogurt, sardines, and fortified plant milks helps regulate the constriction and relaxation of blood vessels. The synergy between these minerals creates a nutritional environment conducive to healthy blood pressure levels.
Dietary fiber, particularly the soluble type found in oats, apples, and legumes, supports both weight management and blood pressure control through multiple mechanisms. Fiber slows digestion, promoting satiety and reducing overall calorie intake. It also helps moderate blood sugar spikes that can contribute to weight gain. For blood pressure specifically, soluble fiber binds to bile acids in the digestive system, forcing the liver to use cholesterol to create more bile. This process gradually lowers circulating cholesterol levels, reducing plaque formation that can stiffen arteries and elevate blood pressure.
When David incorporated regular walking into his routine, he noticed his blood pressure readings began improving within weeks, even before significant weight loss occurred. Physical activity provides immediate benefits to the cardiovascular system independent of weight changes. Exercise stimulates the production of nitric oxide, a compound that signals blood vessels to relax and widen. This vasodilation effect can lower blood pressure for several hours after a single workout, creating a cumulative benefit with consistent activity.
As fitness improves, the heart becomes more efficient at pumping blood, requiring fewer beats per minute to circulate blood throughout the body. This lowered resting heart rate reduces daily strain on the cardiovascular system. Regular exercise also improves insulin sensitivity, helping to prevent the weight gain commonly associated with insulin resistance. The type of exercise matters less than consistency—whether through brisk walking, swimming, cycling, or strength training, movement becomes medicine for both weight and blood pressure management.
Strength training deserves particular attention for its dual impact on metabolic health and blood pressure. While cardiovascular exercise provides immediate blood pressure benefits, resistance training builds lean muscle mass that increases resting metabolic rate. This metabolic boost helps maintain weight loss over the long term. Contrary to outdated concerns about weightlifting spiking blood pressure, properly performed resistance training with controlled breathing actually improves overall cardiovascular function and contributes to lower resting blood pressure readings.
Beyond diet and exercise, lifestyle factors create the context in which weight and blood pressure management either flourish or falter. Sleep represents an often-overlooked component of this equation. Chronic sleep deprivation disrupts hormones that regulate appetite, often increasing cravings for high-calorie foods while reducing motivation for physical activity. Simultaneously, poor sleep keeps the nervous system in a heightened state of alertness, maintaining elevated blood pressure throughout the night instead of allowing the natural dip that occurs with quality rest.
Stress management proves equally crucial to both weight and blood pressure control. During stressful periods, the body releases cortisol and adrenaline—hormones that historically prepared humans for immediate physical action. In modern life, these biochemical signals often have no physical outlet, instead contributing to emotional eating and fat storage, particularly around the abdomen. Chronic stress keeps blood pressure elevated through constant activation of the sympathetic nervous system. Techniques like meditation, deep breathing, and mindful movement can interrupt this cycle, creating space for healthier choices.
Alcohol consumption requires careful consideration in the weight-blood pressure equation. While moderate red wine consumption has received attention for potential heart benefits, excessive alcohol intake provides empty calories that contribute to weight gain while directly raising blood pressure. Alcohol can interfere with blood pressure medications and stimulate appetite, leading to increased food consumption. For those managing both weight and hypertension, limiting alcohol to moderate levels or eliminating it entirely often produces significant improvements in both areas.
Environmental factors, from food accessibility to neighborhood walkability, create the backdrop against which individual choices play out. People living in food deserts without access to fresh produce face greater challenges in maintaining a blood-pressure-friendly diet. Those in neighborhoods without safe walking paths or recreational facilities struggle to incorporate regular physical activity. Recognizing these structural barriers helps explain why some individuals find weight and blood pressure management particularly difficult, highlighting the need for both personal strategies and community-level solutions.
Technology has introduced new tools for managing weight and blood pressure simultaneously. Smart scales that measure body composition provide more meaningful data than weight alone, tracking changes in muscle mass versus fat mass. Wireless blood pressure monitors allow for convenient tracking of readings at different times of day, revealing patterns that single measurements miss. Mobile applications can sync data from both types of devices, helping users visualize the connection between lifestyle choices and their health metrics. These technological aids create accountability and motivation when progress feels slow.
Perhaps the most challenging aspect of managing weight and blood pressure involves navigating the plateaus that inevitably occur. After initial success, the body adapts to new eating patterns and exercise routines, slowing further progress. During these periods, consistency becomes more important than dramatic changes. Small adjustments—increasing vegetable intake by one serving daily, adding five minutes to walks, or practicing stress reduction techniques—can restart progress when more drastic measures prove unsustainable. The gradual nature of improvement in both weight and blood pressure requires patience and recognition that small, consistent actions create significant change over months and years.
Maria discovered this truth after her weight loss stalled three months into her health journey. Rather than abandoning her efforts, she focused on maintaining her new habits while adding short bursts of intensity to her walks. Over the next two months, her blood pressure continued to improve even as the scale moved slowly, demonstrating that health benefits accumulate beyond what numbers alone can capture. Her experience highlights that weight and blood pressure management constitute a marathon rather than a sprint—a lifelong practice of making choices that support cardiovascular health.
The relationship between weight management and blood pressure control represents one of the most well-established connections in preventive medicine. By understanding how nutrition, physical activity, and lifestyle factors influence both simultaneously, individuals can develop integrated approaches that deliver greater benefits than targeting either concern in isolation. The journey requires education, patience, and self-compassion—recognizing that occasional setbacks don't define the overall trajectory. As research continues to reveal new dimensions of this relationship, the fundamental truth remains: small, consistent steps toward healthier living create ripple effects that extend far beyond any single measurement.

By /Oct 14, 2025

By Daniel Scott/Oct 14, 2025

By /Oct 14, 2025

By Thomas Roberts/Oct 14, 2025

By /Oct 14, 2025

By /Oct 14, 2025

By Amanda Phillips/Oct 14, 2025

By Thomas Roberts/Oct 14, 2025

By /Oct 14, 2025

By /Oct 14, 2025

By /Oct 14, 2025

By Megan Clark/Oct 14, 2025

By /Oct 14, 2025
By /Oct 14, 2025

By /Oct 14, 2025
By John Smith/Oct 14, 2025

By Ryan Martin/Oct 14, 2025

By Benjamin Evans/Oct 14, 2025

By /Oct 14, 2025

By /Oct 14, 2025