In the dimly lit corridors of global health governance, a quiet revolution is unfolding. It is a revolution that pits the cold precision of silicon against the warm unpredictability of human spirit, where algorithms meet empathy in a delicate dance that will define the future of human wellbeing. As we stand at this crossroads, the fundamental question emerges: can technology and humanity not merely coexist but synergize to create a more equitable global health landscape?
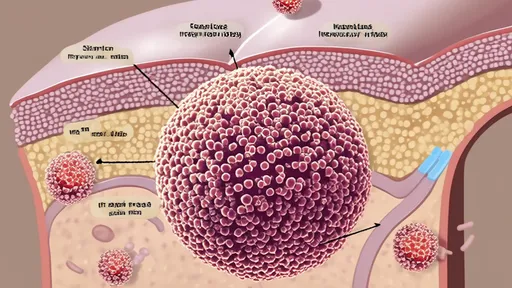
The recent pandemic served as both a crucible and a catalyst, accelerating the integration of digital technologies into global health systems at an unprecedented pace. Contact tracing apps became ubiquitous overnight, AI-powered diagnostic tools processed medical images with superhuman accuracy, and blockchain-enabled supply chains promised unprecedented transparency in vaccine distribution. The technological promise seemed limitless – faster detection, more efficient responses, data-driven decision making. Yet beneath this gleaming surface, troubling questions began to emerge about who these systems truly served.
In rural clinics across sub-Saharan Africa, health workers found themselves grappling with sophisticated diagnostic apps that required constant internet connectivity – a luxury in regions where electricity remains intermittent. The very communities most vulnerable to health crises were being left behind by the digital revolution meant to protect them. This technological divide revealed itself not as a mere technical challenge, but as a profound ethical dilemma at the heart of global health governance.
The architecture of global health governance itself is undergoing a tectonic shift. Traditional institutions like the World Health Organization now find themselves navigating a landscape populated by tech giants, digital health startups, and non-traditional actors wielding data as their primary currency. This new ecosystem brings both promise and peril – the innovative capacity of Silicon Valley coupled with governance models that prioritize shareholder value over public health equity.
At the core of this transformation lies the fundamental tension between technological efficiency and human dignity. Automated triage systems can process patients faster than any human team, but they risk reducing human suffering to data points. Predictive analytics can forecast disease outbreaks with remarkable accuracy, but they raise troubling questions about privacy and surveillance. The very tools designed to save lives could inadvertently erode the human values that make life worth living.
Perhaps the most poignant illustration of this tension emerges from the field of mental health. Digital therapeutics and AI-powered counseling platforms offer the promise of accessible care to millions who would otherwise go untreated. Yet these same technologies struggle to replicate the healing power of human connection – the shared glance, the comforting touch, the unspoken understanding that forms the bedrock of therapeutic relationships. The most advanced algorithm cannot truly comprehend the complex tapestry of human emotion and experience.
The governance challenge becomes even more complex when we consider the global dimension. Data sovereignty concerns have emerged as a major flashpoint, with developing nations rightly questioning why their health data should flow to servers in Silicon Valley or Shenzhen. The patterns extracted from this data become valuable intellectual property, creating a new form of digital colonialism where the global south provides raw data while the global north reaps the commercial benefits.
Yet for all these challenges, examples of hopeful synthesis are emerging. In rural India, community health workers are using simple mobile applications that work offline, designed specifically for low-resource settings. In Brazil, participatory digital platforms are enabling marginalized communities to have a direct voice in health policy decisions. These approaches demonstrate that technology need not be imposed from above, but can be co-created with communities to serve their specific needs and contexts.
The philosophical underpinnings of this synthesis matter deeply. Global health governance must evolve beyond seeing technology as merely a set of tools to be deployed. Instead, we must cultivate what might be called technological humility – an approach that recognizes both the power and limitations of digital solutions, that prioritizes human wellbeing over technological sophistication, that understands that the most elegant algorithm is worthless if it fails to serve the most vulnerable.
This requires reimagining the very metrics by which we measure success in global health. Rather than focusing solely on efficiency gains or cost savings, we must develop frameworks that capture more nuanced outcomes – community trust, cultural appropriateness, psychological safety. A vaccination campaign that reaches 95% of the population through coercive digital surveillance cannot be considered successful if it erodes public trust in health institutions.
The path forward demands nothing less than a new social contract for digital health – one that establishes clear ethical boundaries, ensures equitable benefit sharing, and centers human dignity in technological design. This contract must be global in scope but locally responsive, recognizing that the same technology that empowers communities in one context might oppress them in another.
As we look to the future, the integration of artificial intelligence and machine learning presents both extraordinary opportunities and existential questions. AI systems can analyze vast datasets to identify disease patterns invisible to human researchers, potentially revolutionizing preventive medicine. Yet these same systems risk encoding and amplifying the biases present in their training data, potentially creating self-perpetuating cycles of health inequality.
The most promising developments are those that embrace what might be called augmented intelligence rather than artificial intelligence – systems designed to enhance human decision-making rather than replace it. These approaches recognize that the wisdom of experienced healthcare workers, the intuition of community leaders, and the lived experience of patients represent forms of knowledge that cannot be reduced to algorithms.
Global health governance stands at a pivotal moment. The choices we make today about how to integrate technology while preserving humanity will reverberate for generations. We must navigate this path with both bold vision and profound caution, remembering that the ultimate measure of our success will not be the sophistication of our technologies, but their ability to serve human flourishing in all its beautiful complexity.
In the final analysis, the most important technological innovation may be the simplest – systems that listen as well as they compute, that understand context as well as data, that recognize the human story behind every statistic. The future of global health depends not on choosing between technology and humanity, but on weaving them together in service of a world where every person can experience health not merely as the absence of disease, but as the presence of human dignity.

By /Oct 14, 2025

By Daniel Scott/Oct 14, 2025

By /Oct 14, 2025

By Thomas Roberts/Oct 14, 2025

By /Oct 14, 2025

By /Oct 14, 2025

By Amanda Phillips/Oct 14, 2025

By Thomas Roberts/Oct 14, 2025

By /Oct 14, 2025

By /Oct 14, 2025

By /Oct 14, 2025

By Megan Clark/Oct 14, 2025

By /Oct 14, 2025
By /Oct 14, 2025

By /Oct 14, 2025
By John Smith/Oct 14, 2025

By Ryan Martin/Oct 14, 2025

By Benjamin Evans/Oct 14, 2025

By /Oct 14, 2025

By /Oct 14, 2025