In the quiet corridors of palliative care units, a profound transformation occurs daily—not in the eradication of disease, but in the meticulous art of symptom management and comfort care. This specialized approach to medicine represents a fundamental shift from curative treatments to holistic support, where the quality of life becomes the central focus. The philosophy underpinning this care model recognizes that even when a cure is no longer possible, there remains an immense capacity for healing—healing defined not by laboratory results but by human dignity, comfort, and peace.
The journey begins with comprehensive symptom assessment, a process requiring both clinical expertise and profound human connection. Healthcare professionals in palliative care develop an almost intuitive understanding of their patients' needs, recognizing that unexpressed pain often speaks through subtle cues—a tightened jaw, restless movement, or withdrawal from interaction. This nuanced observation forms the foundation of effective symptom control, where the goal extends beyond mere numerical pain scales to the restoration of personal autonomy. Patients are encouraged to articulate their experiences in their own terms, creating a collaborative partnership in care that honors their unique perspectives and preferences.
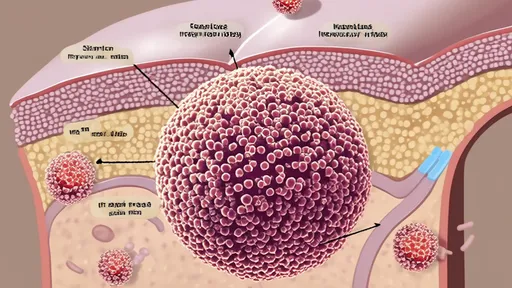
Pain management constitutes the cornerstone of palliative symptom control, yet it represents one of the most complex challenges in medical practice. The subjective nature of pain demands individualized approaches that consider not only physical sensations but emotional and spiritual dimensions as well. Modern palliative care has moved beyond the traditional fear of opioid medications, embracing balanced protocols that prioritize patient comfort while minimizing side effects. The sophisticated use of adjuvant medications—including antidepressants, anticonvulsants, and local anesthetics—has revolutionized pain control, allowing for targeted relief of neuropathic and bone pain that often proves resistant to conventional analgesics.
Beyond pharmacological interventions, integrative therapies have gained significant recognition for their role in comprehensive pain management. Techniques such as therapeutic massage, acupuncture, and mindfulness meditation work in concert with traditional medicine to address the multifaceted experience of suffering. These modalities recognize that pain exists within a context of personal history, cultural beliefs, and emotional states, requiring approaches that engage the whole person rather than isolated symptoms. The evidence supporting these complementary therapies continues to grow, demonstrating their capacity to reduce medication requirements while enhancing overall well-being.
Respiratory symptoms present particularly distressing challenges for patients with advanced illness, with dyspnea—the subjective experience of breathlessness—ranking among the most frightening sensations a person can endure. The palliative approach to respiratory distress combines pharmacological management with environmental and psychological support. Opioids, carefully titrated to individual need, can remarkably reduce the sensation of air hunger without suppressing respiratory drive to dangerous levels. Meanwhile, simple interventions like positioning, fan therapy, and breathing techniques empower patients to regain a sense of control over their breathing, transforming panic into manageable rhythm.
The management of nausea and vomiting requires similar sophistication, as these symptoms may stem from multiple causes including metabolic disturbances, medication side effects, gastrointestinal obstruction, or increased intracranial pressure. Palliative specialists employ a systematic approach to identify the underlying mechanisms, selecting antiemetic medications that target specific neurotransmitter pathways. The strategic combination of drugs working through different mechanisms often proves more effective than single-agent therapy, reflecting the complex neurophysiology of nausea. Additionally, non-pharmacological approaches such as aromatherapy, acupressure, and dietary modifications provide valuable adjuncts to medical treatment.
Perhaps the most overlooked aspect of symptom management involves addressing fatigue and weakness, which profoundly impact quality of life yet often receive less attention than more dramatic symptoms. The palliative approach to fatigue recognizes it as a multidimensional phenomenon involving physical, psychological, and spiritual dimensions. Energy conservation techniques, strategic rest periods, and gentle mobilization exercises help patients preserve function while accepting necessary limitations. This balanced approach avoids both the frustration of unrealistic expectations and the resignation of complete inactivity, instead helping patients find meaningful engagement within their changing capacities.
Comfort care extends far beyond symptom control to embrace the environmental, psychological, and spiritual dimensions of the human experience. The physical environment plays a crucial role in patient well-being, with attention to lighting, noise control, temperature, and personal space creating a sanctuary for healing. Family photographs, favorite music, and cherished objects transform clinical spaces into personal territories, reinforcing identity and continuity amid the disruptions of illness. These seemingly small details carry profound significance, serving as anchors to normalcy and sources of comfort when medical interventions reach their limits.
Skin care and hygiene represent fundamental components of comfort that transcend mere cleanliness to become expressions of human dignity. Meticulous attention to pressure ulcer prevention, oral care, and personal grooming communicates respect for the individual beyond their medical condition. The simple act of washing becomes an opportunity for human connection and gentle touch, providing comfort that words cannot express. Specially trained palliative care nurses develop expertise in managing complex wounds and skin conditions, using advanced dressings and positioning techniques to prevent and treat breakdown while maximizing patient comfort.
Nutritional support in palliative care requires careful consideration of competing priorities—the symbolic importance of food, the pleasure of eating, and the practical realities of declining intake. Rather than aggressively pursuing artificial nutrition in advanced illness, palliative teams help patients and families navigate the emotional landscape of changing eating patterns. The focus shifts from nutritional targets to the experience of eating itself, emphasizing comfort, pleasure, and social connection. Small, appealing meals, attention to food preferences, and creative adaptations to swallowing difficulties honor the role of food in human relationships while respecting the body's natural progression.
Psychological and emotional support forms the invisible architecture of comfort care, addressing the fear, anxiety, and depression that often accompany serious illness. Specially trained social workers and psychologists provide therapeutic support using modalities adapted to the unique needs of palliative patients. Life review techniques help individuals find meaning and coherence in their personal narratives, while cognitive-behavioral approaches address specific fears about death and dying. The creation of legacy projects—whether through recorded messages, written materials, or artistic expressions—allows patients to continue their presence in the lives of loved ones, addressing the fundamental human need for continuity beyond physical existence.
Spiritual care, provided by professional chaplains or spiritual care providers, attends to questions of meaning, purpose, and transcendence that arise with particular intensity at life's end. This dimension of care remains fully inclusive, serving patients of all religious traditions and those with no formal spiritual affiliation. Through deep listening and presence, spiritual caregivers help individuals explore their understanding of life's ultimate concerns, finding peace with unfinished business and reconciling relationships. Rituals, prayers, or simple ceremonies often provide structure for expressing what words cannot capture, creating containers for profound emotional and spiritual experiences.
Family support represents an essential extension of comfort care, recognizing that serious illness affects entire networks of relationships. Palliative teams provide education, emotional support, and practical assistance to family caregivers, who often navigate complex medical landscapes while managing their own grief and exhaustion. Respite care, counseling, and support groups help sustain caregivers through the prolonged journey of illness, recognizing that their well-being directly impacts patient comfort. When death approaches, families receive guidance about what to expect and how to provide comfort, transforming fear into meaningful participation in their loved one's final moments.
The final days and hours of life demand particularly specialized comfort measures, with attention turning exclusively to peaceful transition. Symptom management intensifies to ensure freedom from distress, while unnecessary monitoring and interventions are discontinued to preserve the dignity of the natural dying process. Environmental modifications—soft lighting, familiar voices, gentle touch—create an atmosphere of sacred peace. The expertise of palliative teams shines most brightly in these moments, as they guide families through the mysterious territory of active dying, normalizing the process while honoring its profound significance.
In reflecting on the comprehensive nature of symptom management and comfort care, we recognize that this approach represents medicine at its most humanistic. The sophisticated integration of pharmacological science, psychological insight, and basic human compassion creates a tapestry of support that honors the whole person. Rather than representing medical failure, palliative care demonstrates healthcare's capacity to accompany patients through life's most challenging transition with expertise, respect, and profound compassion. The true measure of this care emerges not in prolonged survival, but in the quality of moments—the comfort of a pain-free hour, the peace of reconciled relationships, the dignity of maintained personal control, and the profound connection between caregiver and patient that transcends the boundaries of life itself.

By /Oct 14, 2025

By Daniel Scott/Oct 14, 2025

By /Oct 14, 2025

By Thomas Roberts/Oct 14, 2025

By /Oct 14, 2025

By /Oct 14, 2025

By Amanda Phillips/Oct 14, 2025

By Thomas Roberts/Oct 14, 2025

By /Oct 14, 2025

By /Oct 14, 2025

By /Oct 14, 2025

By Megan Clark/Oct 14, 2025

By /Oct 14, 2025
By /Oct 14, 2025

By /Oct 14, 2025
By John Smith/Oct 14, 2025

By Ryan Martin/Oct 14, 2025

By Benjamin Evans/Oct 14, 2025

By /Oct 14, 2025

By /Oct 14, 2025